I found out the hard way what it looks like when Cambridge’s Accident and Emergency Department at Addenbrooke’s (which actually covers a much greater geographical area) it hit by an unexpected, unseasonal spike in admissions
For those of you wondering why I hadn’t blogged for almost a week, it was because I got stuck in our city’s hospital in the middle of a capacity crisis. Which meant I got to see how it coped from the inside. Furthermore, because staff cannot speak out publicly over these things, I promised them that I’d do it for them. So thank you to the staff on wards EAU3 and C5 for putting up with me, and A&E plus the paramedics (again) for processing me!
Also, apologies in advance to any politicians and senior execs who are about to get deluged with public questions, queries, moans, and rants coming from my direction
In a nutshell I was woken up at 5.30am with pains on my arm that reminded me of the last time I was admitted to Addenbrooke’s. What I thought and hoped would be a straight-forward series of blood tests at A&E early in the morning followed by a decision to admit or discharge, ended up taking far longer than it should have done – although not for the fault of the staff at Addenbrooke’s. What I’m talking about is an institutional and structural problem – one that is also Political. Highly Political.
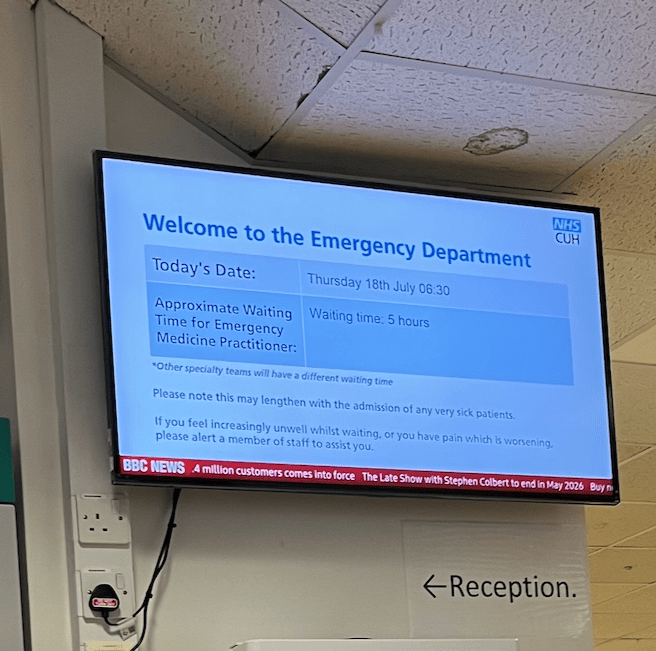
Above – in A&E with the photo time-stamped at 7:58am showing the approximate waiting time to see a senior physician following the series of tests that patients in the waiting room have to go through
The maximum length of waiting to be seen is four hours. At the time of writing, demand remains high in A&E at Addenbrooke’s – see their page explaining what happens and why there are still long waiting times here.
When the main test results I was interested in came back with the ‘all clear’, (something that actually took far, far longer than it should have done given that the waiting time subsided a few hours later) I assumed I was going to be out by the early afternoon. But given my history and the fact the pains remained unexplained, they kept me in for further tests. Given how busy things were by then, I said I was happy to come back as an outpatient but they insisted I stick around. But there was a problem. There were no spare beds available.
“How on earth does Addenbrooke’s run out of beds?!?”
Sadly this is not a new phenomenon, nor is it as rare as it should be. The refusal of successive chancellors and health secretaries to approve funding to expand the hospital’s district-level services to match the expansion of Cambridge (whose population has grown by 50% since I started secondary school in the early 1990s) means that, along with an ageing population the demand regularly outstrips supply.
Addenbrooke’s Accident and Emergency deals with 4 times the volume of people it was designed for was what I wrote in December last year. Just over six months later I got to see what it looked like when A&E had to deal with over twice as many admissions as it was designed to cope with – its last expansion being in 2001.
Thus I found myself staying overnight not in a bed, but in a reclining chair with a handful of fellow patients in a similar position in ward EAU3 which is a quieter, more comfortable waiting area normally for those waiting to be discharged after initial treatment. The problem was that with such crowding in the main A&E waiting area, they had to send as many of us up to this floor to ease the pressure.
“Wasn’t it all irresponsible teenagers getting drunk and ending up in hospital? It was Friday night after all!”
The older staff told me that today’s generation of teenagers are not the drunken hell-raisers that my generation was in the 1990s, and that anecdotally they get fewer levels of teenage drunkeness than in the run-up to the Millennium. One of the big challenges comes with an ageing population and the increased risk of accidents in the home resulting in hospital admissions – something of a built environment retrofitting challenge for public policy-makers.
I found the news of over 150 people still being in A&E in the early hours – far beyond the capacity of what it was designed for, to be utterly astonishing.
There were about a dozen of us who spent the night on big reclining chairs being kept entertained by a continental European healthcare assistant called Milo, who must have spent half the night making us teas and coffees while me and a couple of other patients tried to come up with ideas on how to overhaul things in and around our city.
Addenbrooke’s as a microcosm of an international city
For anyone who has been admitted to hospital can tell you, you spend most of your time waiting. And watching. And listening. What hospital environments do due to a variety of ultimately Political decisions, is they bring together a huge diverse group of people who would otherwise never choose to work with the same group of people in the same place at the same time – and under the same huge pressures for such little financial return. It’s something that few outside a healthcare setting perhaps understand, and perhaps even fewer within academia have studied from a sociological perspective.
If you want to have the best healthcare in the world, you have to be open to employing the best staff – from all over the world
As with previous admissions, there was this curious mix that no private sector corporation would consciously put together to solve some of the most difficult and challenging problems in society: people in poor health in great need with multiple problems/challenges.
- Fairly-recent school leavers who like me grew up locally, going to the same schools and colleges as friends and family
- Young 20-something doctors/physicians with very sharply-polished RP accents
- Apprentice healthcare assistants from Eastern Europe
- Specialist technical staff from South America
- Qualified nurses from India and South-East Asia
- Trainee pharmacists from Commonwealth Africa fluent in multiple languages
- Civic society volunteers – both students on charity placements and local middle-aged residents running charity libraries and book lending services
- Long term White working class porters with an untapped in-depth knowledge of what the challenges are at the hospital
And how good are our ‘future of Cambridge’ consultations at engaging with such diverse audiences who can not only speak about their own needs, but also speak about the needs of the most vulnerable in our society? Here’s what happened last time.
Such was the scale of the unexpected peak that Addenbrooke’s simply did not have the capacity to get the further tests done that I was originally kept in for
One of the first things you find out about in A&E is the concept of ‘clinical need’ – and that those with the most urgent and acute needs get seen before others. Given the limited capacity, that meant me moving lower down the list. But when you are sharing a ward bay with half a dozen other patients, more than half of whom are very ill indeed, human empathy kicks in. In such situations my disposition tends to be:
- The last thing in the world healthcare staff need me to be is a difficult patient – their job is hard enough as it is. Or as I often say to healthcare professionals looking after me: ‘My job is to make your job as easy as possible. Tell me what I need to do and I’ll do it. I trust in your skills, training, and profession’
- Let that more ill person go before me – I’m in no rush. It’s even more hard-hitting when they have a shell-shocked next-of-kin who is reluctant to leave the side of an ill loved one for a moment.
On the second point, I have a sort-of empathy gap the root of which is a mix of my neurodiverse disposition and my CFS/ME diagnosis. Much as I’d love to have ended up in a position of being in a long-term relationship with roots back to college/university years, for a whole host of reasons it didn’t happen. At the same time, ever since I went down with CFS post-2012, I have really struggled to function in the company of other human beings. The idea of sat next to the same person in the same place hour after hour, day after day, I don’t know who would drive the other person mad first! Chronic fatigue changes you, and forces you to reassess so many things in life that you previously took for granted.
Instead of being out by Monday lunchtime, it wasn’t till Wednesday early evening that I was finally discharged
…and the Post-Exertional Malaise was brutal! I don’t think I left the house on Thursday, and only managed to crawl out of bed on Friday if only to pick up some more meds. (I wanted to go to the picket line to support the doctors’ strike at Addenbrooke’s earlier today, having supported their previous actions in times gone by).
So if I owe you an email or a completed task, please accept my apologies for the unforeseen delay!
If you are interested in the longer term future of Cambridge, and on what happens at the local democracy meetings where decisions are made, feel free to:
- Follow me on BSky
- Spot me on LinkedIn
- Like my Facebook page
- Consider a small donation to help fund my continued research and reporting on local democracy in and around Cambridge.

